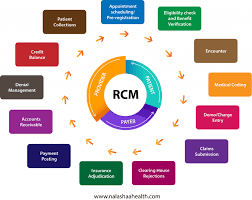
Several industry standards and guidelines exist to provide frameworks and best practices for RCM implementation, such as those from organizations like the Society for Maintenance & Reliability Professionals (SMRP) and the International Organization for Standardization (ISO). ...
Read more